Antidepressant medications provide crucial support for millions battling depression. Yet for some, use can cross the line into antidepressant addiction. With a staggering 400% increase in antidepressant use between 2005-2008, understanding the signs of dependence and how to help is more critical than ever. Read on
Understanding Antidepressant Addiction
Antidepressant addiction is a complex issue that differs from addiction to substances like alcohol, opiates, or cocaine in several key ways. Understanding these differences is essential for effectively recognizing and addressing antidepressant addiction.
How Antidepressant Addiction Differs from Other Addictions
- Lack of euphoria: Unlike opioids or cocaine, antidepressants do not produce a euphoric high.
- No cravings: People taking antidepressants do not typically experience the intense drug cravings common in other types of addiction.
- No negative consequences: Antidepressant addiction does not usually involve negative consequences like job loss or relationship problems, which are often associated with other addictions.
Antidepressant addiction, while a real phenomenon, differs significantly from addictions to other substances. The lack of euphoria, cravings, and negative consequences often associated with drug abuse sets it apart. However, it’s crucial to recognize that antidepressants addiction is a legitimate issue that requires proper management and care from healthcare professionals.
Types of Antidepressant Addiction
There are two main types of antidepressant addiction:
- Physical dependence: This occurs when the body adapts to the presence of the antidepressant and experiences withdrawal symptoms when the medication is stopped or reduced.
- Psychological dependence: Less common, this type of addiction involves an emotional attachment to the antidepressant, with the person feeling that they need it to function or cope with life.
Side Effects of Antidepressant Addiction:
The side effects of antidepressant addiction can include:
- Withdrawal symptoms: Abruptly stopping antidepressants may lead to symptoms such as nausea, hand tremors, and depression.
- Misuse: Some people may attempt to abuse antidepressants by snorting them, but this does not typically lead to addiction.
- Co-occurring disorders: People with depression are more likely to abuse other drugs, which can worsen depression symptoms and interfere with the effectiveness of antidepressants.
In summary, while antidepressant addiction differs from other addictions in terms of euphoria, cravings, and negative consequences, it can still lead to physical and psychological dependence and withdrawal symptoms when use is abruptly discontinued.
Identifying Antidepressant Addiction and Withdrawal Symptoms
Antidepressant addiction is a chronic disease marked by psychological addiction and physical dependence. Common signs of antidepressant dependence include:
- Taking higher doses than prescribed
- “Doctor shopping” for multiple prescriptions
- Experiencing withdrawal when stopping medication
Signs of Use vs. Addiction
| Antidepressant Use | Antidepressant Addiction |
| Taking medication as prescribed | Increasing dosage without medical approval |
| Storing medication securely | Hiding or stockpiling medication |
| Attending regular doctor check-ins | “Doctor shopping” for multiple prescriptions |
| Tapering off slowly under supervision | Inability to cut back despite desire to do so |
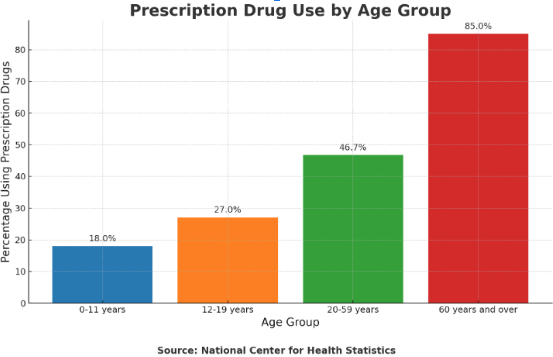
Antidepressant withdrawal symptoms affect 4-7% of users and can mimic other conditions, leading to misdiagnosis. However, antidepressants are just one type of prescription drug widely used in the United States, especially among certain age groups, as shown in the following chart:
This data highlights the widespread use of prescription drugs, providing context for understanding the potential prevalence of antidepressant use and the risk of developing dependence or experiencing withdrawal symptoms.
Symptoms include:
- Nausea and vomiting
- Hand tremors
- Worsened depression
- Brain “zaps” or electric shock sensations
Initial Steps to Address Antidepressant Dependence
If you suspect a loved one is struggling with antidepressant addiction, it’s essential to approach the situation with compassion and understanding. Here are some initial steps to take:
Expressing Concern
- Choose a time when both you and your loved one are calm and free from distractions
- Express your concerns without judgment, using “I” statements to focus on your own observations and feelings
- Be prepared for defensiveness or denial, and remain patient and supportive
Encouraging Professional Help
- Suggest speaking with a trusted healthcare provider about concerns
- Offer to help find a qualified addiction specialist or treatment center
- Volunteer to accompany your loved one to appointments for support
Discussing Tapering Plans
- Encourage your loved one to work with their doctor on a gradual tapering plan to minimize withdrawal symptoms
- Emphasize the importance of medical supervision during the tapering process
- Offer to help keep track of dosages and schedules if needed
Remember, antidepressant discontinuation syndrome is a serious medical issue, with 50% of users experiencing withdrawal when stopping. A compassionate, supportive approach is crucial in helping your loved one take the first steps towards recovery.
Comprehensive Treatment Options
Overcoming antidepressant addiction requires a multifaceted approach that addresses both the physical and psychological aspects of dependence. A comprehensive treatment plan often includes a combination of Medically Supervised Detox, addiction counseling, and support groups.
Medically Supervised Detox :
Antidepressant detox is the first step in the recovery process, focusing on safely managing withdrawal symptoms as the body adjusts to the absence of the medication. A medical professional may recommend a tapering process, which involves gradually reducing the antidepressant dosage over time.
This approach allows the brain to adapt and minimizes the risk of severe withdrawal symptoms by gradually reducing the antidepressant dosage over time. The tapering schedule will be tailored to the individual, considering factors such as:
- Type of antidepressant
- Duration of use
- Personal health factors
Medically supervised detox offers several benefits:
- Proper monitoring and support
- Intervention if complications arise
- Opportunity to address co-occurring medical or psychiatric conditions that may have contributed to the addiction
Undergoing detox under medical supervision enables individuals to safely navigate the withdrawal process and lay the foundation for the next stages of recovery.
Addiction Counseling
Once the initial detox phase is complete, addiction counseling plays a crucial role in helping individuals address the psychological and emotional factors that contribute to antidepressant dependence. Cognitive-behavioral therapy (CBT) is a commonly used approach that helps individuals identify and change negative thought patterns and behaviors that perpetuate addiction.
Through CBT, individuals learn to:
- Recognize and manage emotional triggers
- Develop healthy coping strategies
- Build the skills necessary to maintain long-term recovery
Other therapeutic approaches, such as motivational interviewing and contingency management, may also be incorporated to enhance treatment outcomes.
Addiction counseling also provides a safe space for individuals to process any underlying traumas, mental health issues, or life stressors that may have initially led to the use of antidepressants. By addressing these root causes, individuals can develop a more comprehensive understanding of their addiction and work towards building a strong foundation for lasting recovery.
Support Groups
Support groups are a valuable component of comprehensive treatment for antidepressant addiction. Sharing experiences with others who have faced similar struggles can help reduce feelings of isolation, shame, and stigma that often accompany addiction.
These groups provide:
- A sense of community and belonging
- Encouragement, accountability, and practical advice for navigating the challenges of recovery
Participants can:
- Learn from the successes and setbacks of others
- Gain new perspectives on their own journey
- Develop a network of supportive relationships
Support groups come in various forms, including:
- 12-step programs like Narcotics Anonymous (NA) and Alcoholics Anonymous (AA)
- Non-12-step alternatives like SMART Recovery and Secular Organizations for Sobriety (SOS)
- Online support forums and groups
Emerging Treatment Options
As research into antidepressant addiction continues to evolve, new tools and approaches are emerging to support personalized recovery plans. One promising development is the use of withdrawal risk calculators, which take into account an individual’s unique factors, such as the type and duration of antidepressant use, to estimate the likelihood and severity of withdrawal symptoms.
These calculators can help healthcare providers and individuals make more informed decisions about the tapering process, potentially reducing the risk of complications and improving the chances of successful discontinuation. However, more research is needed to validate the accuracy and clinical utility of these tools.
Other areas of ongoing research include:
- The development of new medications to treat antidepressant withdrawal symptoms
- The exploration of alternative therapies like mindfulness-based interventions and neurofeedback training to support recovery
“While more research is needed, preliminary tools like withdrawal risk calculators offer hope for personalized antidepressant addiction recovery plans.”
By combining medically supervised detox, addiction counseling, support groups, and emerging treatment options, individuals struggling with antidepressant addiction can access a comprehensive and tailored approach to recovery. This holistic strategy addresses the complex physical, psychological, and social factors that contribute to addiction, providing the necessary support and tools for long-term success.
Building Resilience on the Road to Recovery
Recovery is rarely linear. Past withdrawal heightens future risk, so coping with antidepressant withdrawal effects long-term is key.
Strategies to build resilience:
- Cultivate a strong support network
- Develop healthy self-care routines
- Celebrate milestones (e.g. 1 month, 6 months sober)
- Reframe slip-ups as learning opportunities
Managing antidepressant withdrawal is a marathon, not a sprint: With persistence and support, long-term recovery is possible.
Supporting Loved Ones Through Addiction
Supporting a loved one through antidepressant addiction can be challenging, but your love and encouragement play a crucial role in their recovery. Here are some ways to offer support:
- Educate yourself about antidepressant addiction and recovery to better understand their experience
- Celebrate their progress and milestones, no matter how small
- Encourage healthy habits and self-care practices
- Be a listening ear without judgment
- Attend family therapy or support group meetings to show your commitment to their recovery
- Plan sober, fun activities together to help them build a fulfilling life outside of addiction
Remember, recovery is a journey with ups and downs. Your consistent support and understanding can make all the difference in your loved one’s healing process.
Navigating Relapses
Relapses, or a return to drug use after a period of abstinence, are a common part of the recovery journey. Understanding their nature is key to providing ongoing support.
If a relapse occurs:
- Seek medical attention for any unusual or severe symptoms
- Ensure the person has nearby support to maintain safety
- Activate their predetermined support network, including friends, doctors, or counseling services
Reframe relapses as learning opportunities to identify triggers and adjust management strategies. Multiple attempts may be needed to find the right long-term approach.
Self-Care for Caregivers
As a caregiver, it’s essential to prioritize your own well-being to avoid burnout and maintain the strength to support your loved one. Some self-care tips include:
- Set healthy boundaries and communicate your needs clearly
- Make time for activities that bring you joy and relaxation
- Practice stress management techniques like deep breathing, meditation, or exercise
- Seek support from friends, family, or a therapist to process your own emotions
- Attend caregiver support groups to connect with others who understand your experiences
- Remind yourself that your loved one’s addiction is not your fault or responsibility to fix
By taking care of yourself, you’ll be better equipped to provide the loving support your loved one needs on their path to recovery.
“As we navigate the diverse landscapes of mental health, the silent sentinels—our caregivers—also bear the brunt, underscoring the universal need for self-preservation.”
Legal and Ethical Considerations in Addiction Recovery
Supporting individuals through addiction recovery involves navigating a complex web of legal and ethical considerations. Understanding these issues is crucial for providing effective support and ensuring the best possible outcomes.
Legal Protections for Individuals in Recovery
Federal laws like the Americans with Disabilities Act (ADA) and the Rehabilitation Act offer protection against discrimination for those in recovery from substance use disorders (SUDs).
These laws differentiate between current and former illegal drug users, extending protections to individuals who have completed or are participating in a treatment program. Service providers may use drug tests to verify that former illegal drug users are no longer using.
Ethical Guidelines for Addiction Treatment Professionals
Addiction treatment professionals adhere to a set of core ethical principles, including:
- Informed consent
- Competence and established theory
- Confidentiality
- Duty to warn
- Respect for diverse personal and cultural values
These guidelines help professionals navigate ethical dilemmas and provide the highest standard of care for their clients.
Legal and Ethical Challenges in the Criminal Justice System
Individuals with SUDs often face legal issues stemming from their addiction, which can complicate their recovery journey. Rehabilitation programs play a vital role in addressing these challenges by providing support and targeting the underlying addiction.
Ethical Considerations in Caring for People with Addictions
Providing care for individuals with addictions is ethically complex, involving issues of respect, confidentiality, and justice. Clinicians must strike a delicate balance between honesty and empathy, while also considering the potential harm to others and the impact of addiction on co-occurring health conditions.
The Role of Bioethics in Addiction
Bioethics has played a significant role in deepening our understanding of the ethical dimensions of SUDs, including the impact of stigma, the importance of social support, and the value of harm reduction approaches. Fostering an ethical culture that supports recovery efforts is essential for tackling the multifaceted challenges of addiction.
“Cultivating an ethical culture that supports recovery efforts is crucial for navigating the legal and ethical complexities surrounding addiction.”
By staying informed about these legal and ethical considerations, individuals in recovery and their support networks can more effectively navigate the challenges of addiction treatment and contribute to a more supportive and inclusive environment for all those affected by SUDs.
The Road Forward
Antidepressant addiction is a complex challenge, but recovery is possible with the right support. If you or a loved one are struggling, know that you are not alone. Reach out for help today and take the first step towards healing.
FAQs
1. How can I tell if someone is addicted to antidepressants?
Potential red flags include increased dosage, seeking prescriptions from multiple doctors, and withdrawal symptoms when stopping. However, only a medical professional can formally diagnose addiction.
2. What is the typical timeline for antidepressant withdrawal?
Antidepressant withdrawal timelines vary based on factors like medication type and length of use. On average, acute symptoms peak in the first week and subside within 1-3 months. However, some may experience protracted symptoms for several months or longer.
3. Where can I find support for myself as a caregiver?
Consider antidepressant addiction therapy options for yourself, such as counseling or caregiver support groups. Organizations like Al-Anon and the National Alliance for Caregiving provide resources and meetings. Remember, caring for yourself enables you to best care for your loved one.
4. What legal protections are available for individuals in recovery from addiction?
The Americans with Disabilities Act (ADA) and the Rehabilitation Act provide protection against discrimination for individuals in recovery from substance use disorders (SUDs). These laws differentiate between current and former illegal drug users, extending protections to those who have completed or are participating in a treatment program.
5. What are some core ethical guidelines for addiction treatment professionals?
Addiction treatment professionals adhere to a set of core ethical principles, including informed consent, competence and established theory, confidentiality, duty to warn, and respect for diverse personal and cultural values. These guidelines help professionals navigate ethical dilemmas and provide the highest standard of care for their clients.
6. How can rehabilitation programs help individuals with SUDs facing legal issues?
Individuals with SUDs often face legal issues stemming from their addiction, which can complicate their recovery journey. Rehabilitation programs play a vital role in addressing these challenges by providing support and targeting the underlying addiction.
7. How long does antidepressant detox typically take?
The length of antidepressant detox can vary depending on factors such as the specific medication, duration of use, and individual health considerations. Generally, a gradual tapering process is recommended, which can take several weeks to several months, depending on the starting dosage and the rate of reduction.
8. Is it necessary to attend addiction counseling if I’ve already completed detox?
Yes, addiction counseling is a crucial component of comprehensive treatment for antidepressant addiction. While detox addresses the physical aspects of dependence, counseling helps individuals identify and address the underlying psychological and emotional factors that contribute to addiction. Attending counseling sessions can provide the tools and support necessary for long-term recovery.
9. Can I attend support groups even if I’m not religious or comfortable with the 12-step approach?
Absolutely. While 12-step programs like Narcotics Anonymous (NA) and Alcoholics Anonymous (AA) are well-known, there are many alternative support groups available that do not have a religious or spiritual focus. Options like SMART Recovery and Secular Organizations for Sobriety (SOS) provide a more secular approach to peer support, while online forums and groups offer accessible support for those who may have difficulty attending in-person meetings.
10. What are the key signs to watch for if I’m concerned about relapse into antidepressant addiction?
Relapse into antidepressant addiction can be subtle, with key signs including a resurgence of symptoms the medication originally treated, expressed desires to increase dosage without medical advice, isolating behaviors, and any unauthorized changes in medication regimen. Recognizing these signs early and consulting with healthcare professionals can help prevent a full relapse and adjust the recovery plan as needed.