If you or a loved one have ever experienced bedsores, you know firsthand the pain and discomfort they can cause. Bedsores, also known as pressure ulcers, are a common problem for individuals who are bedridden, using a wheelchair or have limited mobility. These painful wounds can be stubborn and difficult to treat, but fortunately, you can use various tips and tricks to manage and treat bedsores effectively.
This article will explore some of the most effective methods for treating bedsores, providing you with the tools you need to take control of this debilitating condition and start healing. Whether you are a caregiver or an individual at risk of developing bedsores, these tips will help minimize pain and promote healing.
What are Bedsores?
Bedsores don’t develop because a person woke up on the wrong side of the bed – it’s because they’ve been stuck in the same position in the bed every day.
Bedsores, also known as pressure ulcers or pressure sores, develop due to lasting pressure on specific body areas. These are injuries to the skin and underlying tissue that result from prolonged pressure on the skin. They often develop in people who are bedridden or have limited mobility and can occur on any part of the body that is subjected to pressure, such as the hips, heels, and back.
Bedsores typically begin as red, inflamed areas that can progress to open wounds if left untreated. They can be painful and increase the risk of infection. These sores are treatable, but complete healing isn’t always possible. Bedsores are a serious medical condition that requires prompt treatment, as these can grow large and, in some instances, become life-threatening. Steps should be taken to prevent their development in people who are at risk.
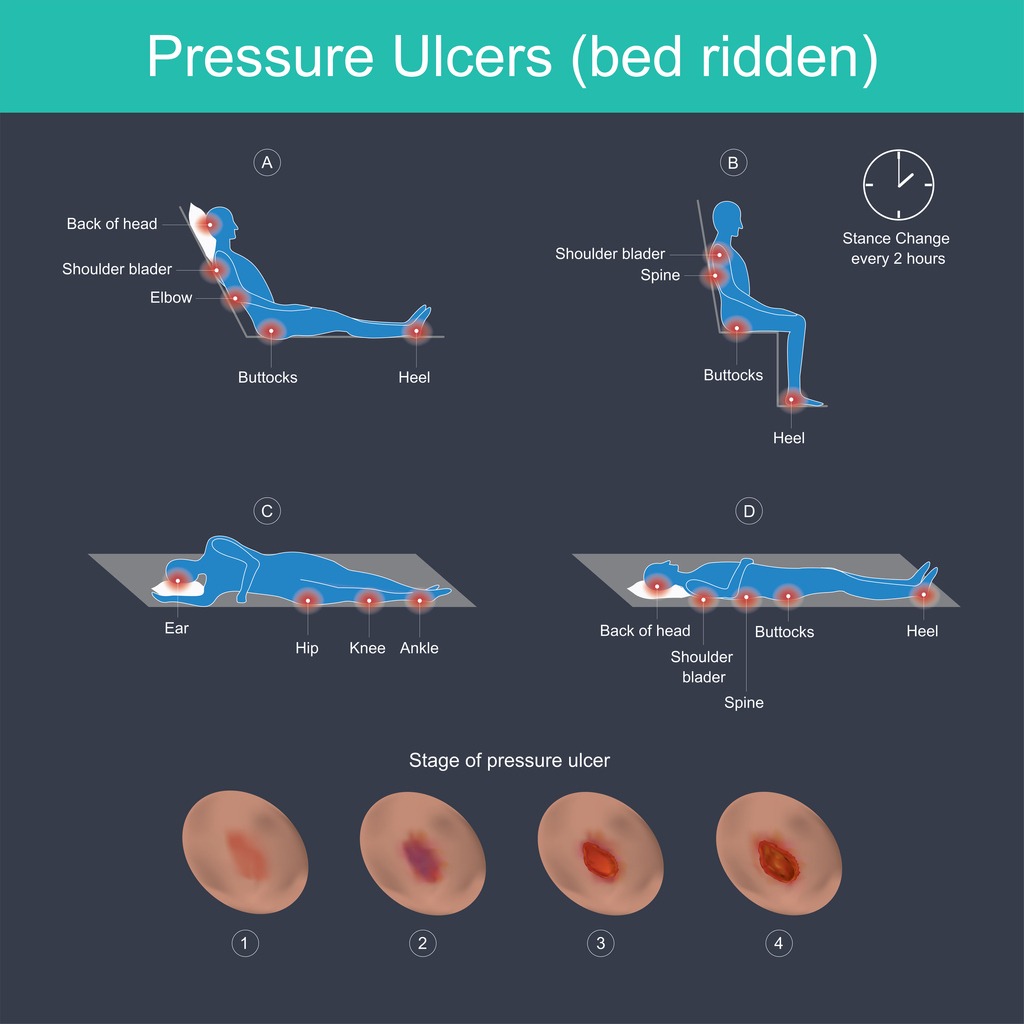
What Parts of the Body Do Bedsores Affect?
Bedsores can affect any part of the body, but it most likely develops on the parts of the body where the bones sit closest to the skin.
A person who spends a lot of time sitting, like those using a wheelchair, may develop sores on the:
- Buttocks
- Tailbone
- Spine
- Shoulder blades
- Back of the legs or arms
A bedridden person may develop sores on the:
- Back
- Shoulders
- Tailbone
- Elbows
- Heels
- Ankles
- Back of the head
- Buttocks
While these mentioned body parts are the typical problem areas targeted by bedsores, they can also develop in unconventional areas. For example, people who use oxygen therapy may develop pressure sores on the bridges of their noses, the back of their heads, or their ears. Bedsores can also form inside the mouth due to ill-fitting dentures, intubations, or mechanical ventilation.
What are the Causes of Bedsores?
Bedsores develop when there is prolonged pressure on the skin, which can cause a reduction or complete cut-off of blood flow to the affected area. This lack of blood flow can lead to the development of a pressure wound injury in as little as two hours, causing skin cells on the epidermis, or the outer layer of skin, to die. As the dead cells break down, a pressure ulcer injury forms.
In addition to pressure, bedsores are more likely to develop in the presence of sweat, urine, or stool moisture. Traction, which is the pulling or stretching of skin that can occur when sliding down in an inclined bed or wheelchair, can also contribute to the development of bedsores. It is important to be aware of these contributing factors and take appropriate measures to prevent the development of bedsores in individuals who are at risk.
Who is at Risk for Bedsores?
People who have limited or no ability to move and those with thinner skin are more likely to develop bedsores: These include people who:
- Use wheelchairs
- Are bedridden due to a medical condition
- Are in a coma or a vegetative state
- Have spinal cord injury
- Experience paralysis
- Wear casts, splints, or other prosthetic devices
- Have poor blood circulation
- Are malnourished and dehydrated
- Have a low or high body mass index (BMI) – either of which can increase pressure
- Have low body weight, as they have less padding for their bones
- Are older, as skin becomes thinner and more fragile
- Have incontinence, which increases the risk of infection and skin damage
Children and adults with certain health conditions are more likely to develop bedsores, including:
- Cancer
- Dementia
- Diabetes
- Kidney failure
- Heart failure
- Cerebral palsy
- Chronic venous insufficiency
- Malnutrition
- Peripheral artery disease
What are the Symptoms of Bedsores?
The symptoms of bedsores can vary depending on the severity of the wound, but common signs and symptoms include the following:
- Skin discoloration – Light skin may turn pink or red or darken. Dark skin may become purplish, bluish, or shiny. If the discoloration doesn’t disappear after removing pressure for 10-30 minutes, this may indicate that bedsore has formed.
- Broken skin – There may be an open, shallow sore with pus or fluid in it.
- Texture changes – The affected area may feel spongy, hard, or warm.
- Infection – Signs of infection include oozing pus, green or black tissue around the sore, change in color, and sensation around the edge of the sore, as well as fever and chills.
- Pain or tenderness in the affected area
- Swelling or inflammation
- A warm or cool sensation in the skin around the sore
- An open wound or ulcer that is slow to heal
- Pus-like drainage or an unpleasant odor
- The formation of a scab or crust over the wound
- A depression or indentation in the skin
How are Bedsores Diagnosed?
Bedsores are typically diagnosed through a physical examination by a healthcare professional. The healthcare provider will examine the affected area and check for signs of skin damage, including redness, swelling, and open wounds.
In some cases, a healthcare provider may use additional diagnostic tests to determine the extent of the damage and whether an infection is present. These tests include:
- Tissue biopsies
- Blood culture and tests
- X-rays
- MRIs
It is essential to seek medical attention immediately if you or someone you care for is experiencing symptoms of bedsores. Early diagnosis and treatment can help prevent the development of more severe complications and promote healing.
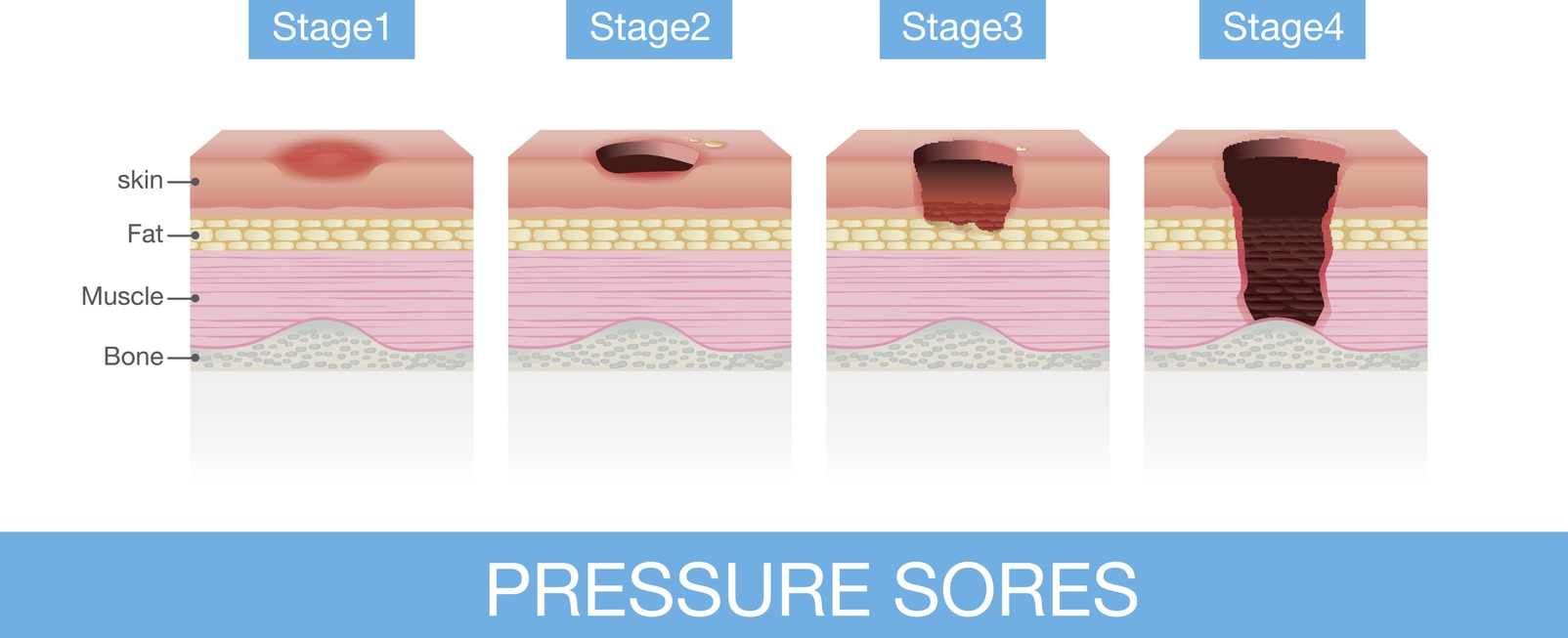
What are the Stages of Bedsores?
There are different levels of severity of a pressure ulcer. Healthcare providers use this staging system to apply the proper treatment. Stages of bedsores include:
1. Stage 1
This is the mildest stage, as these pressure sores only affect the upper layer of the skin. For light-colored people, the skin looks red or pink, and there is no open wound. For people with darker skin, it may be hard to see a color change. The affected area may also be firmer or softer, warmer or cooler than the surrounding skin, and may not blanch or turn white when pressed.
Your healthcare provider may call this stage a pressure injury. With proper care and treatment, stage 1 bedsores can often be managed and prevented from progressing to more severe stages.
Treating a stage 1 bedsore typically relieves pressure on the affected area and keeps the wound clean and protected. Here are some tips for treating a stage 1 bedsore:
- Relieve pressure – The first step in treating a bedsore is to relieve pressure on the affected area. This may involve changing positions frequently, using specialized support surfaces such as cushions or mattresses, and avoiding tight clothing or bedding that can compress the skin.
- Keep the wound clean – Clean the affected area with mild soap and water and pat dry. Avoid rubbing or scrubbing the area, as this can further irritate the skin.
- Protect the wound – Apply a thin layer of protective barrier cream or ointment to the affected area to prevent further skin damage and promote healing.
- Monitor for progression – Check the affected area daily for any color, size, or texture changes. If the wound is getting worse or not healing, seek medical attention promptly.
A stage 1 pressure sore can be healed in as little as two to three days.
2. Stage 2
A stage 2 bedsore is a pressure injury that has progressed beyond the initial stage and involves damage to the skin’s deeper layers. The affected area may appear as an open wound, blister, or shallow crater at this stage. The surrounding skin may also be discolored and feel warm or tender to the touch. The skin forms an open sore, and the area around it may be red and irritated. It may ooze clear fluid or pus, and it’s painful.
Stage 2 bedsores typically involve damage to the skin’s epidermis and dermis layers. They may take several weeks to heal with proper treatment.
Treating a stage 2 bedsore involves managing the wound and promoting healing. Besides the treatment protocols listed above, you may need to manage pain when it comes to stage 2 bedsores. Over-the-counter pain relievers or prescription pain medications may be necessary if the wound is painful.
A stage 2 pressure sore should get better in a matter of days to three weeks.
3. Stage 3
A stage 3 bedsore is a pressure injury that has progressed further and involves damage to the skin and tissue beneath it. The sores may have gone through the skin’s fatty layer or the hypodermis. At this stage, the wound may appear as a deep crater with a visible fat layer, and the surrounding skin may be discolored and have a tough, leathery texture. You may be able to see the body fat in the ulcer. The wound may also have a foul odor and may be painful.
Treating a stage 3 pressure ulcer requires specialized medical care and attention. Besides removing pressure and keeping the wound clean, here are some general steps that may be taken to treat it:
- Undergo debridement – The damaged tissue in and around the wound must be removed, a process called debridement. This can be done through surgical means, such as with a scalpel or with specialized dressings that help remove the dead tissue.
- Dress the wound – Cover the affected area with a sterile dressing or bandage to protect it from further damage and promote healing. Various dressings may be used depending on the wound’s size, depth, and drainage.
- Manage pain – If the wound is painful, over-the-counter pain relievers or prescription pain medications may be necessary.
- Take antibiotics –In cases where the wound is infected or at risk of infection, antibiotics may be prescribed to prevent or treat the infection.
- Improve nutrition – Proper nutrition is critical for healing bedsores. A diet rich in protein and other nutrients can help promote healing and prevent further damage.
- Get specialized care – Depending on the severity of the wound, specialized care such as vacuum-assisted closure or skin grafting may be necessary.
A stage 3 pressure sore may take at least a month and up to several months to heal.
4. Stage 4
A stage 4 bedsore is the most severe type of pressure injury. The wound at this stage has penetrated all three layers of the skin. Some may even affect the muscles and ligaments. At this stage, the wound is deep and may have a large, open crater with exposed bone or muscle visible.
The surrounding skin may be discolored, thickened, or have a leathery texture. The wound may also have a foul odor and may be extremely painful. In some cases, there may be signs of infection, such as fever, chills, and increased drainage from the wound.
Prompt and appropriate treatment prevents further damage, complications, and even death. Stage 4 bedsores are treated in the same way done for stage 3 bedsores, with more options considered, such as:
- Surgery – Depending on the severity of the wound, surgery may be necessary to repair the damaged tissue, close the wound, or graft healthy tissue onto the affected area.
- Specialized care – Depending on the individual case, specialized care such as negative pressure wound therapy or hyperbaric oxygen therapy may be necessary.
A stage 4 bedsore could take anywhere from three months or longer. It may even take years to heal.
How to Prevent Bedsores
If you or your loved one is at risk of developing bedsores, here are some steps that can be taken to prevent it:
- Change position – The primary cause of bedsores is pressure on the skin, so it’s important to relieve pressure on bony areas of the body, especially for those who are bedridden or have limited mobility. This can be done by changing positions frequently, between every 15 minutes to every two hours if you’re in bed. If you’re immobile, ask a caregiver to help you reposition yourself.
- Check the skin regularly – Monitor the skin regularly for any signs of redness, discoloration, or changes in texture. If you notice any changes, take action immediately to relieve pressure on the affected area.
- Keep skin clean and dry – Moisture on the skin can increase the risk of bedsores, so it’s essential to keep the skin clean and dry. This can be done using gentle cleansers and moisturizers and regularly changing wet or soiled clothing or bedding.
- Use the right cushion – Specialized cushions and mattresses, such as pressure-relieving mattresses or cushions, can help reduce the risk of developing bedsores. Do not use donut-shaped cushions, as they reduce blood flow to the area.
- Encourage movement – Regular movement can help improve circulation and reduce the risk of developing bedsores. Encourage those with limited mobility to change positions frequently or to perform exercises that can be done while sitting or lying down.
- Maintain a healthy diet – Proper nutrition is important for maintaining healthy skin and preventing bedsores. A diet rich in protein and other nutrients can help promote healing and prevent further damage.
- Quit smoking – Smoking can impede circulation and increase the risk of developing bedsores, so quitting smoking is important in preventing bedsores.
If you are always sitting, here are some ways to prevent bedsores on the buttocks: